David Uttley can almost pinpoint the exact time his nightmare began. He was 15 and on holiday in Brittany.
“I fell asleep in the sun on the beach. I couldn’t walk the next day. The sunburn was so painful.” Today, at 60, she is living with stage four melanoma cancer.
Like many men growing up in the Sixties, Seventies and Eighties, he knew little about sun protection.
“I would be sent out to play in the garden without any protection. I can’t blame my family, it was unthinkable at the time,” he says. “But the damage had already been done and once it’s done it can never be repaired.”
Skin cancer rates in the UK are at an all-time high, with a sharp increase among over-55s. Melanoma, the most dangerous form of skin cancer, reached 17,500 cases last year, the highest number since records began. The increase has been particularly pronounced among over-50s, which has been attributed to the boom in cheap package holidays in the 1960s. Case rates in this age group have risen by 195% since the 1990s, with more men than women affected.
Experts predict a similar backlash from Gen Xers, the sun worshippers who blushed at Costas as he sang George Michael’s “Don’t Worry, You Can Sunbathe”.
Uttley’s story is a sobering one. In 2013, aged 49, he noticed a ‘bum mole’ on his shoulder. It was diagnosed as malignant melanoma. After surgery, he was discharged and told to regularly check his lymph nodes (neck, groin, armpit) for lumps.
“It was almost an accident on my part,” he says.
In 2017, she found a lump in her armpit and had her lymph nodes removed. “Melanoma loves soft tissue, and the lymphatic system provides a highway around your body. It can go anywhere it wants, and when it gets there, it parties,” Uttley says.

She had regular scans and became well acquainted with ‘scan anxiety’ – the nervous wait between scans and results. In 2020, a routine scan discovered cancer was partying in her pancreas. Surgeons removed it and her spleen.
Today, she is living with stage four cancer, waiting to see where and when the disease will strike next. In the meantime, she is an ambassador for Melanoma UK and raised £20,000 for the charity when she climbed Kilimanjaro in 2023. She will climb again in December this year and is raising money through a GoFundMe page.
“A stage four diagnosis makes it much more real and focuses your mind on your own mortality,” she believes.
He has seen many cancer patients die. “I always say I am lucky, my story is a walk in the park compared to some of the poor souls I have met.”
Uttley uses his story as a warning to others and sees a tsunami in the distance.
“People are so indifferent to the sun and don’t really understand the damage that UV rays can do. Skin cancer isn’t taken that seriously,” Uttley says. “It’s just skin cancer, right? That’s what they say. Cut it out and you’ll be fine. That’s a huge misconception.
“The attitude of men towards sun damage is appalling. You see all these construction workers standing outside in the heat, naked in the sun. I feel sorry for them. There are so many risks and they have no idea.”
Studies show that getting a sunburn once every two years triples your risk of developing skin cancer compared to never getting a sunburn.
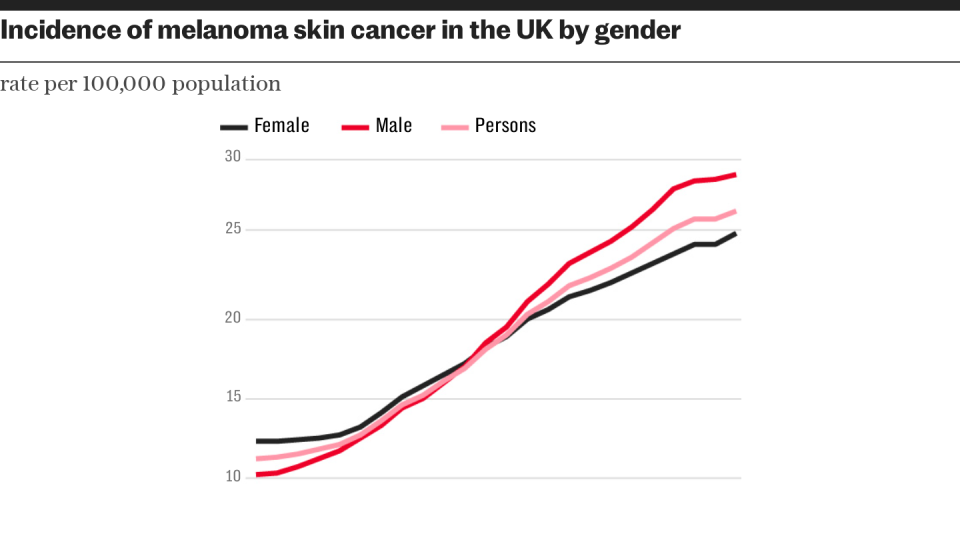
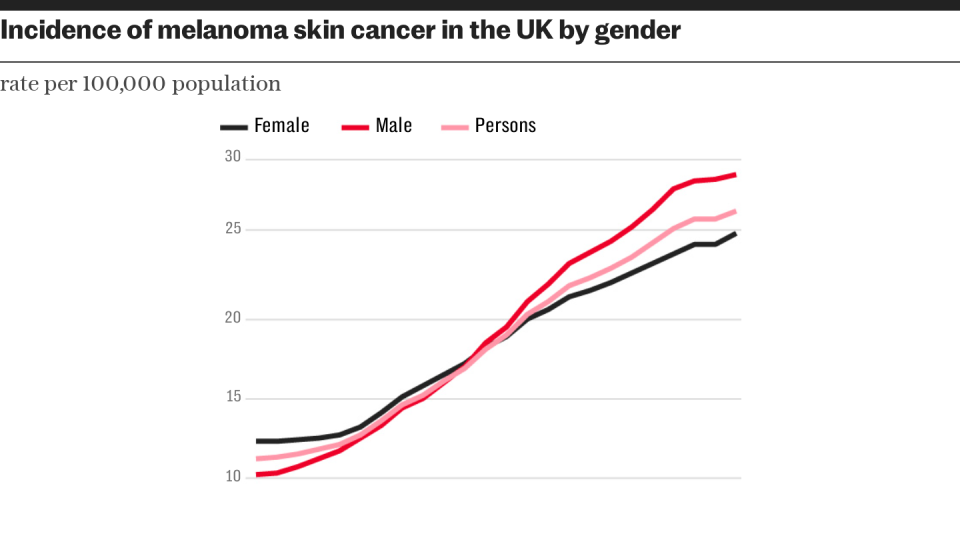
Melanoma rates in Britain have risen by almost a third across all age groups in the past decade, with researchers predicting a record 20,800 cases this year. Men are more likely to develop melanoma than women by the age of 50, and women are twice as likely to develop melanoma by the age of 65, according to the American Academy of Dermatology.
Dr Paul Banwell, former head of the East Grinstead Melanoma and Skin Cancer Unit and now runs the Banwell Clinic, said: “Over the last decade, the rate of melanoma skin cancer in men in the UK has increased significantly more than the rate of cancer in women.
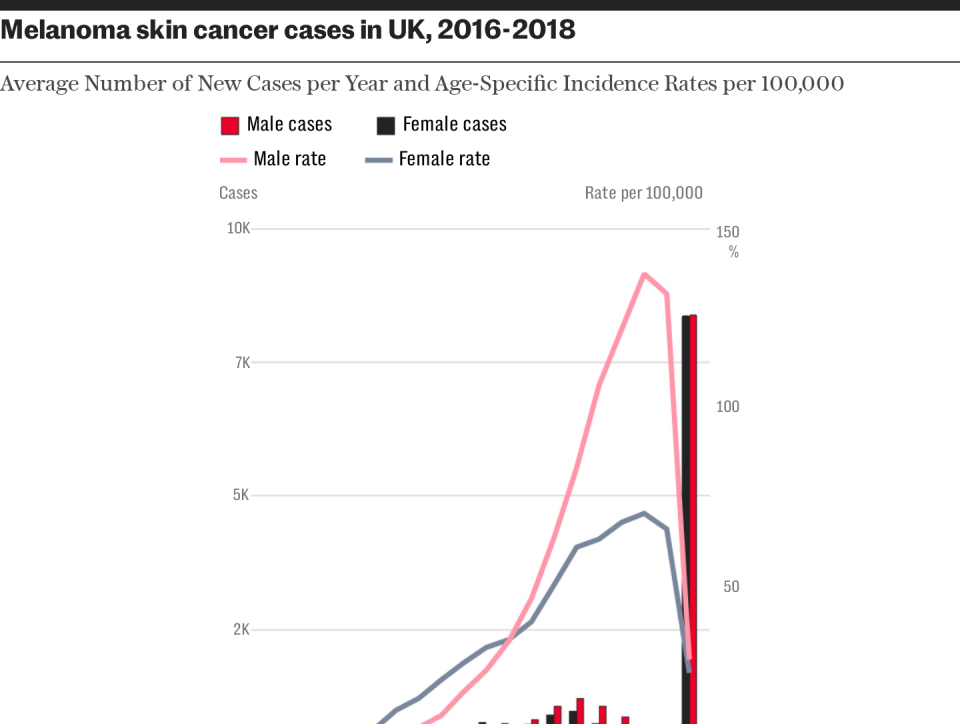
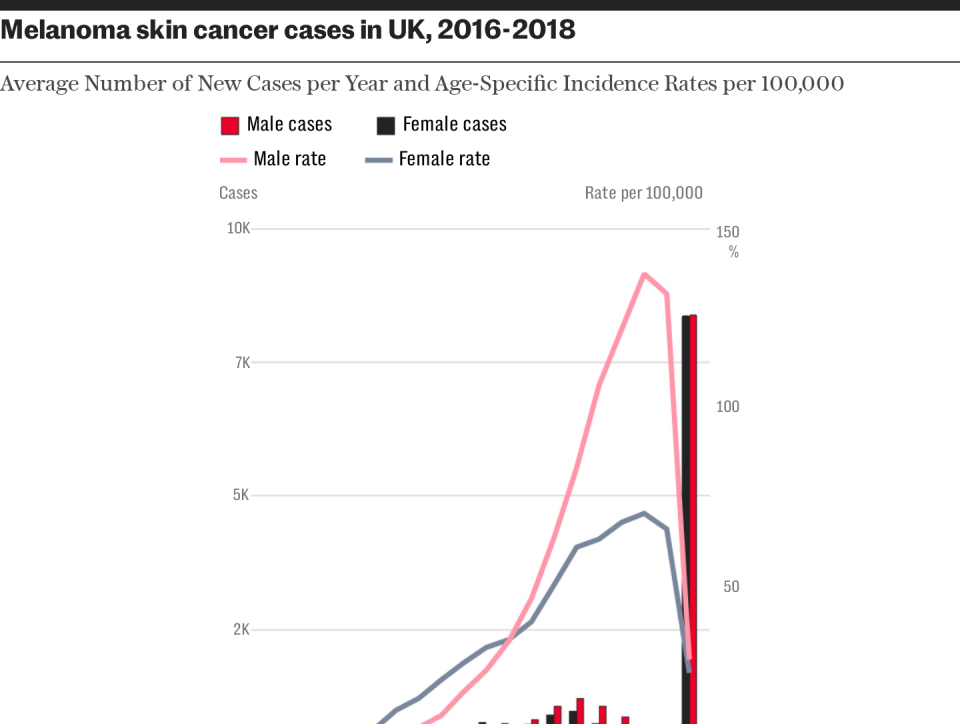
“There has been an alarming 8% increase in death rates in men. Skin cancer is not only on the rise in men, it is also more common in men. Men are also more likely to be diagnosed at a later stage and are more likely to die from melanoma than women.”
Uttley laments British attitudes to sun care.
“There’s a completely different ethos in Australia or Brazil. There are sunscreen dispensers everywhere and there’s a common-sense attitude that if you expose your skin without protection, you’re tempting your fate,” he says.
But despite better awareness, melanoma is still the most common cancer among 15 to 39-year-olds in Australia. More than 14,000 people are diagnosed each year, and two in three people in the Oceania nation will develop skin cancer in their lifetime. According to John Thompson, emeritus professor of melanoma and surgical oncology at the University of Sydney, more than 50 per cent of Australian adults will have had at least one skin cancer by the time they are 50.
“It’s a complex story,” says Prof. Thompson. “There is an epidemic of melanoma, particularly in older men, and this reflects attitudes towards sun care decades ago.”
Today in Australia, awareness of sun damage and UV protection begins in primary school and continues through to high school. Primary school children cannot go outside without wearing a hat, and playgrounds and sports fields are designed with covered shaded areas.
“Parents are very aware of the risk to young children,” says Prof. Thompson. “Children are protected from birth and this continues through kindergarten and school. Workplaces are also very aware – some provide sunscreen containers and outdoor workers are encouraged to use it and wear protective clothing such as hats and long-sleeved shirts.”
Employers are being held liable and many people are being sued by workers who developed melanoma from working outdoors and not being provided with proper sun protection.
In Australia, sun protection messages have been part of the public health landscape since the 1980s, when the Slip, Slop, Slap campaign was launched, advising citizens to wear a shirt, sunscreen and a sun hat.
Attention was again heightened after a three-part television documentary was broadcast in 1987. Goodbye Sunabout a young man who died of melanoma. In the three months since publication, there has been a 167% increase in the number of melanoma diagnoses compared to the same period the previous year. More recently, the country has banned tanning beds.
Despite all the public messaging, Australia still tops the global list for skin cancer, even though rates have stabilised. Part of the reason for this, says Prof Thompson, is that “by the time people get into adolescence and early adulthood, when they leave school, they think they are invincible”. In a country of beaches, the allure of a tan is too much for many.
Jay Allen is trying to change that.
In 2008, at age 32, Allen was diagnosed with stage 3 melanoma. In January 2021, after being cancer-free for more than 12 years, she found a golf ball-sized lump on the right side of her neck. It was diagnosed as squamous cell carcinoma, for which Allen underwent radiation and chemotherapy. This month, she was given the all-clear.
Allen is the chief executive and founder of the Australian Skin Cancer Foundation, which she set up in 2021 to raise awareness and provide advocacy education and support. It operates a free mobile skin cancer screening service. The side of the NGO’s skin checker features photos of more than 80 friends Allen met through her work who have died of melanoma.
The nurses in the truck see up to 200 people a day, queuing in car parks before the service forms. So far they have checked more than 7,000 people across 52 locations. The service found more than 32 melanomas, more than 600 basal cell carcinomas and more than 700 squamous cell carcinomas.
Allen has just completed a 13-day tour of Queensland, where melanoma rates are among the highest in the world.
The Australian calculates that around 40 per cent of the population are being careful and aware of the risks, “but another 60 per cent still tan and don’t get regular skin checks.”
“Here, tanning and looking good is part of the culture. We should try to change that. There is a lot of education in kindergarten and primary school, but then everything falls apart in high school.”
Skin cancer is a slow-growing disease. The damage is hidden and waiting, and only becomes apparent decades later. The impact of public health messaging in eighties Australia is only now becoming clear, with the incidence curve flattening over the last five to 10 years.
“Public health campaigns appear to have had some impact,” says Prof. Thompson. “While we are plateauing, the United States, Britain and many continental countries are catching up,” he adds.
“For example, within the next decade the incidence of melanoma in the white population in the United States will be about the same as that currently seen in Australia.”
Dr. Banwell adds a sobering note: “Gen X and younger generations seem to be taking sun safety more seriously, but there are also worrisome trends on social media from time to time, like the ‘anti-SPF’ trend or the ‘homemade sunscreen’ trend seen on TikTok. These can be incredibly harmful and have serious consequences as people age.”
And tanning beds are still worryingly popular in the UK. A survey by the charity Melanoma Focus earlier this year found that 28% of Brits aged 16 to 65 used them, compared with 43% of those aged 18 to 25. Around 40% of the 2,000 Brits surveyed were unaware of the risks.
Tanning beds are banned for under-18s in the UK. Chief executive Susanna Daniels said: “The use of tanning beds is alarmingly high across the UK and it is shocking that many people do not realise how dangerous they are.”
Without historical buffers or public health awareness, we are not yet out of the fire in the UK.
How can you protect yourself?
Beth Vincent, health information manager at Cancer Research UK, says: “To reduce your risk, seek shade, especially in the middle of the day, wear a shirt that covers your shoulders, wear a hat and sunglasses, and apply sunscreen of at least SPF 30 and four or five star rating regularly and generously.”
Dr. Banwell adds: “Men need to pay attention to areas that are often overlooked, such as the ears, eyelids, lips, nape of the neck, tops of the feet, and especially the scalp if they are bald.
“It’s also difficult for men to identify and pinpoint areas of concern on their backs and may need to ask a partner for help. I always recommend applying SPF 50.”
Choose a wide-brimmed hat instead of a baseball cap. Women are more prone to sun damage on their lower legs.